Transfer a Mosaic Embryo in IVF: Understanding Fertility, PGT-A (preimplantation genetic testing for aneuploidy) and mosaic embryo transfer options
When you’re going through IVF, every result brings new questions — and one of the most confusing ones is the mosaic embryo. If you’ve been told that one of your embryos has mosaicism, you’re not alone — and it’s completely normal to feel unsure what that means or what to do next.
In this article, we’ll guide you through the essentials: What exactly is a mosaic embryo? How does it differ from normal or aneuploid embryos? And most importantly, should you consider transferring a Mosaic Embryo in IVF?
This is for you if you’re looking for clarity, support, and trustworthy information about mosaic embryo transfer, fertility outcomes, and the options you can consider before moving forward.
What is a mosaic embryo and how does it affect IVF?
Understanding the role of a Mosaic Embryo in IVF is vital for making informed decisions about your fertility journey.
Understanding mosaic embryos and mosaicism in IVF
A mosaic embryo is an embryo that contains both normal and abnormal cells — a situation known as mosaicism. This mix can happen within the same embryo during early development, typically after fertilisation. While some cells are chromosomally normal (euploid), others might have too many or too few chromosomes, which are referred to as aneuploid. Mosaicism does not come from the egg or sperm directly, but from errors that occur during early cell divisions. This type of chromosomal mosaicism in human embryos has been recognised more often in recent years thanks to improved testing methods.
Understanding mosaic embryos means recognising that they are not entirely abnormal. Many embryos identified as mosaic still have the potential to implant and result in healthy pregnancies. In fact, some mosaic embryos have the ability to self-correct or push abnormal cells aside during further development. While the biology is complex, the key point is this: a mosaic embryo is an embryo that is somewhere in between a euploid and a fully abnormal embryo — and that can make things complicated when deciding what to do next.
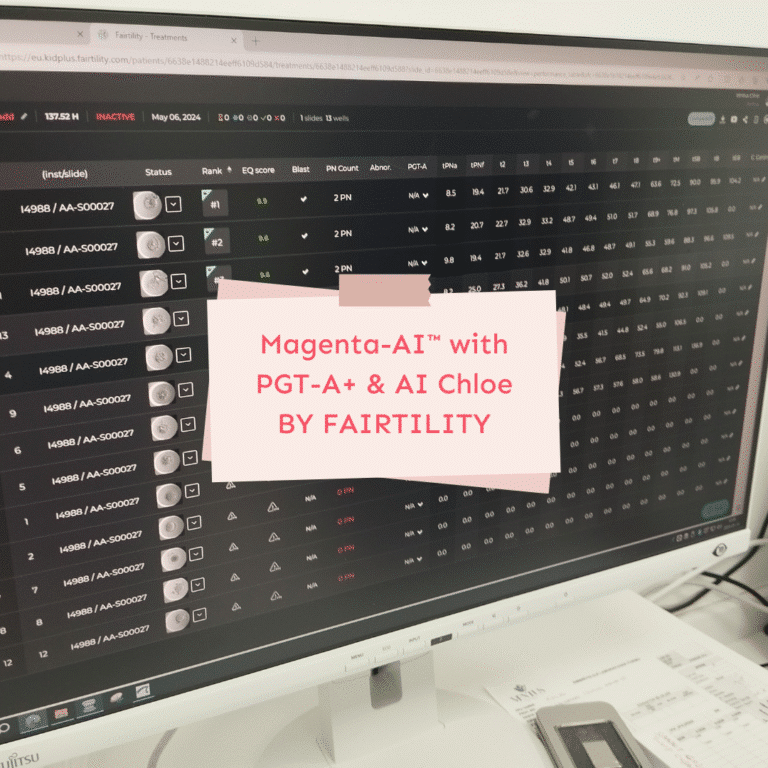
Why mosaic embryos are identified during PGT-A
Thanks to preimplantation genetic testing for aneuploidies (PGT-A), fertility specialists can now detect mosaic patterns more precisely than ever. During an IVF cycle, a small number of cells are taken from the embryo’s outer layer — this is called an embryo biopsy — and analysed for chromosomal structure. If some of those cells are normal and others show irregularities, the embryo is classified as mosaic.
This doesn’t mean that the whole embryo is affected — the inner cell mass, which develops into the baby, might be normal. But since the biopsy only samples a few cells, PGT-A can’t guarantee the overall status. That’s why mosaic embryo results often leave couples in a difficult position, wondering whether a mosaic embryo may still lead to a live birth, or whether a transfer would involve too many unknowns.
It’s also important to remember that embryos are classified as mosaic at different levels. Some have low-level mosaicism, while others show segmental mosaic patterns involving only part of a chromosome. Each type comes with different implications for implantation, pregnancy outcome and the decision to transfer.
What happens after a mosaic embryo is identified?
How embryos are identified as mosaic through preimplantation genetic testing
Once your embryos reach the blastocyst stage during IVF, some clinics offer preimplantation genetic testing (PGT-A) to check for chromosomal irregularities. This process involves carefully removing a few cells from the trophectoderm — the outer layer that later forms the placenta. These cells are then tested to see whether the chromosomes are balanced.
If the sample shows a mix of normal and abnormal cells, the embryo is identified as mosaic. That means the results fall somewhere between euploid (normal) and aneuploid (abnormal). The mosaic result may involve whole chromosomes or just segments — a case of mosaic known as segmental mosaic. Because the sample only represents part of the embryo, it doesn’t give a full picture of what’s happening inside. Still, it’s the best insight available at this stage of IVF.
PGT-A has improved our ability to detect mosaic embryos — but it has also made decisions more complicated. Embryos diagnosed with mosaic results weren’t always visible in earlier years, so many were transferred unknowingly. Now that they are being flagged, we face new questions about whether to transfer a mosaic embryo or wait for a clearer option.
Interpreting mosaic embryo results and next steps in IVF
The first thing to know is: a mosaic embryo is not automatically excluded from transfer. In many cases, it may still be considered for transfer — especially if no euploid embryos are available. However, this is where decision-making becomes personal and emotional. Some couples choose to transfer a mosaic embryo after talking with a fertility specialist. Others prefer to wait for another IVF cycle, or hope for a new euploid embryo.
The actual decision depends on several factors: the level and type of mosaicism, the chromosomes involved, your age, your overall fertility history, and the number of embryos for transfer. It’s also essential to speak with someone experienced in genetic counseling — they can explain what the findings really mean for your pregnancy chances and live birth rate.
Keep in mind: a mosaic embryo may still lead to a healthy baby. Many clinics now agree that embryos with mosaicism — particularly low-level types — should not be discarded automatically. Instead, they can offer another path forward when options are limited. Transferring embryos with mosaic results is a personal choice, but one that deserves careful, compassionate support.
“Sometimes, the hardest part isn’t the treatment itself — it’s making decisions when the answers aren’t black and white. That’s why information and calm support matter so much.”
Nathalie Wiederkehr
Transfer or not? Making decisions around mosaic embryo transfer
What to consider before you transfer a mosaic embryo
One of the hardest moments in an IVF journey is deciding what to do when a mosaic embryo is all that’s left for transfer. After so much waiting, hope and effort, this situation can feel deeply unfair — and yet, it’s one that more and more women face today.
Before you transfer a mosaic embryo, it’s important to understand both the potential and the uncertainty involved. Mosaic embryos have the potential to implant, to grow, and even to result in healthy babies. At the same time, transferring mosaic embryos comes with a slightly lower chance of success compared to transferring a euploid embryo.
What makes things even more complex is that not all mosaic embryos are equal. Some show low-level mosaicism and involve less critical chromosomes. Others may affect areas that are more likely to interfere with implantation or pregnancy development. This is where clinical grading, segmental mosaic patterns, and expert judgment really matter. It’s not a clear yes or no — it’s about context and weighing your options carefully.
If no euploid embryos are available and you’re emotionally and physically ready, many women choose to transfer a mosaic embryo. Others may prefer to try another IVF cycle first. There is no right or wrong choice — only what feels manageable and meaningful for you right now.
The role of genetic counseling in deciding whether to transfer
Genetic counseling is more than just another appointment. It’s a conversation that helps you make sense of what your mosaic embryo result really means. A trained counselor will explain which chromosomes are involved, what types of outcomes are associated with your specific findings, and what your pregnancy chances might look like.
For many women, talking through the risks of transferring mosaic embryos brings unexpected relief. It helps replace the anxiety of the unknown with real information — and makes the decision-making process feel less overwhelming. You may learn, for example, that embryos with low-level mosaicism often lead to successful pregnancies. Or that certain mosaic patterns — like those involving smaller, non-critical chromosomes — are associated with higher success rates and even live birth.
This support is especially important when no euploid embryos are left and you are thinking about whether to transfer a mosaic. Having a space to ask questions, voice your concerns and receive honest answers can change the whole experience. It’s not about removing uncertainty — it’s about giving you the clarity and confidence you need to choose your next step.
Risks and outcomes of transferring mosaic embryos
Understanding the risks of transferring mosaic embryos in IVF
When considering the transfer of a mosaic embryo, the biggest question is often about risk. Are mosaic embryos safe to transfer? What are the chances that something could go wrong? These are normal and valid concerns — especially after all the emotional and physical energy you’ve already invested in your IVF journey.
Embryos with mosaicism do carry a slightly higher risk profile than euploid embryos. The most common risks of transferring mosaic embryos include a reduced implantation rate, a higher chance of miscarriage, and — in rare cases — developmental complications. However, it’s crucial to understand that these risks depend heavily on the specific type of mosaicism involved.
For example, embryos with low-level mosaic patterns or segmental mosaic findings are often associated with better outcomes than those showing high-level or complex abnormalities. Some studies even suggest that embryos as mosaic — especially those involving less critical chromosomes — may behave more like normal embryos than previously thought.
In practice, this means that the risk level is not fixed — it varies depending on how the embryo is classified, which chromosomes are involved, and the overall quality of the embryo. The embryo’s origin matters too: embryos from young egg donors or younger patients may tolerate mosaic variations better than others.
Ultimately, the decision to move forward with a mosaic transfer isn’t just about numbers. It’s about understanding the full picture — the science, the limitations of testing, and the reality that some embryos diagnosed with mosaic results have resulted in perfectly healthy live births.
Success rates, pregnancy chances and fertility outcomes
Despite the uncertainties, mosaic embryos have led to many successful outcomes. While the live birth rate is slightly lower than with euploid embryos, it’s far from zero — and in many cases, still a hopeful option when no other embryos are available. The overall success rates vary depending on the clinic, the type of mosaicism, and the criteria used to prioritise embryos for transfer.
According to the Preimplantation Genetic Diagnosis International Society, the transfer of embryos classified as mosaic should be considered when euploid options are not available — especially if the findings suggest a lower level of abnormal cells. Clinics often develop their own internal guidelines for the prioritisation of mosaic embryos, factoring in age, fertility history, and specific test results.
If you’re transferring embryos with mosaic results, your fertility specialist will help you understand what to expect. In many cases, mosaic embryos result in healthy pregnancies — and sometimes in babies who are genetically confirmed as normal after birth. The key is to have support from a team that respects your emotional landscape as much as your medical one.
Mosaic embryos are not a last resort — they are part of a broader, evolving conversation in modern fertility treatment. With the right information, you can make a calm and informed choice about what’s right for you.
Prioritisation and selection of embryos for transfer
How clinics approach prioritisation of mosaic embryos
When more than one embryo is available for transfer, clinics follow certain guidelines to decide which one to prioritise. In a perfect scenario, a euploid embryo — one with the expected number of chromosomes — is usually the first choice. But in many IVF cases, especially involving egg donation or patients over 40, mosaic embryos are often the only embryos identified as potentially transferable.
Clinics use detailed grading systems based on morphology, PGT-A results and the type of chromosomal irregularity. If a mosaic embryo is the only option, or if no euploid embryos are available, doctors may recommend transferring a mosaic embryo that shows low-level or segmental mosaic patterns. These types tend to be associated with better implantation rates and a higher chance of pregnancy than high-level or complex mosaic findings.
Embryos are classified according to several factors, including the percentage of abnormal cells, the affected chromosomes, and the predicted risk of developmental impact. Clinics also take into account patient age, embryo quality, and previous IVF history. The decision-making process is clinical — but it is also sensitive to your personal situation. Your voice matters just as much as the numbers do.
Comparing euploid and mosaic embryos in IVF
When it comes to outcomes, euploid embryos are generally considered the most likely to lead to a live birth. They have higher implantation potential, lower miscarriage rates, and better overall pregnancy outcomes. But not everyone undergoing IVF will have a euploid embryo available for transfer.
Mosaic embryos sit in a grey zone — they’re not considered ideal, but they are increasingly viewed as viable options. Recent studies have shown that many mosaic embryos result in healthy babies, especially when the level of mosaicism is low or when the embryo shows good development. This is why embryos with mosaic results are no longer automatically excluded from consideration.
Choosing between a euploid embryo and a mosaic embryo (if both are available) may come down to the details. If you have a single euploid embryo of poor quality and a high-quality mosaic embryo, your clinic might even suggest prioritising the mosaic one. In other cases, especially when transferring embryos is already emotionally and physically taxing, some patients choose to transfer the most genetically stable embryo available — regardless of grading.
Either way, what matters most is understanding the facts, the uncertainties, and your own emotional readiness. IVF is not just a medical process — it’s a human one. And with good guidance, even the most difficult choices can become manageable.
What does all this mean for your fertility journey?
Balancing IVF hopes with risks of transferring
Reaching the point where you’re considering a mosaic embryo means you’ve already been through a lot. By now, you’ve probably read lab reports, waited on PGT-A results, and spoken with your clinic more times than you ever imagined. You’ve had hopes rise and fall — and now you’re being asked to weigh your next step carefully.
This is where knowledge about mosaic embryos becomes truly empowering. Yes, the risks of transferring a mosaic embryo are real — but so are the possibilities. Mosaic embryos have led to healthy babies. They have implanted, grown, and brought joy into families where no euploid embryos were available. And importantly, many of these embryos were once thought to be unusable.
Still, it’s okay if the uncertainty feels heavy. Balancing your hope for a baby with the risks of transferring is never easy. No one can guarantee a specific outcome. But with the right support — from your clinic, your fertility specialist, and your own sense of clarity — you can make a choice that feels right for you. That’s what this journey is really about: making informed, gentle decisions at each turn.
When to consider transferring a mosaic embryo
There is no one-size-fits-all answer to whether a mosaic embryo should be transferred. But there are moments when it becomes a real and meaningful option. If you’ve already completed multiple IVF cycles without a euploid result, or if your embryo quality is good despite mosaicism, this might be the embryo that gives you a real chance at pregnancy.
You may also consider transferring a mosaic embryo if your clinic confirms it’s low-level, involving chromosomes that are not typically associated with severe outcomes. Or if you simply feel emotionally ready to move forward without waiting any longer.
Ultimately, choosing to transfer a mosaic is not about settling — it’s about understanding your options deeply and trusting yourself to move ahead. Embryos with mosaicism are not perfect, but they are not hopeless either. In fact, they are part of a growing field of IVF knowledge that reminds us: even with complexity, life finds a way.
Final thoughts and where to go from here
The impact of mosaic embryos on IVF decision-making is still evolving. While they aren’t considered chromosomally normal embryos, they are also not the same as fully abnormal ones. Each mosaic embryo result adds to what we know — and gives us new ways to personalise fertility care.
If a mosaic embryo is identified, it’s natural to feel torn. The decision to transfer a mosaic isn’t simple. You may feel hopeful and hesitant at once — especially if this embryo came from your last cycle. But remember: the use of mosaic embryos is no longer experimental. They are actively being studied, tracked and transferred across clinics worldwide — and in many cases, with positive outcomes.
What happens prior to transfer matters. A good clinic will review your options based on your medical history, your mosaic embryo result, and the embryos before transfer. This includes whether you’ve had embryos during preimplantation sex determination or need clarification on whether you’re dealing with a mosaic aneuploid finding. And yes, even human embryos during preimplantation sex testing can reveal mosaic patterns.
Most importantly: embryos should not be discarded automatically just because they carry some mosaic traits. Many of them — even those associated with mosaic segments — still implant, grow, and result in healthy births. This is why your voice and comfort level count just as much as the science.
If you’re ready to explore your options further, I’ve put together a guide with real, non-promotional insights into clinics across Europe — including where the transfer of mosaic embryos is possible, where preimplantation testing is used transparently, and where support is available in your language.
Ready to explore your options — with clarity and support?
If you’re still unsure what to do next, you’re not alone. That’s exactly why I created a guide to IVF destinations in Europe — including where mosaic embryo transfer, PGT-A and gender selection are possible, and what to expect in terms of success rates and clinic approaches.
You can also book a private 1:1 session if you’d like to talk through your options in a supportive, non-judgmental space. I don’t recommend clinics in general — I help you find the ones that suit your needs best.
Download the guide or book a consultation — so you can move forward with more clarity, and less overwhelm.