The Life of an Embryologist: Understanding Their Vital Role in IVF and Fertility
When we think about IVF, we often picture doctors, medication, or the moment of embryo transfer. Yet behind every successful IVF cycle stands another professional whose work you rarely see but who carries great responsibility – the embryologist. These specialists guide eggs and sperm through the earliest stages of life, making sure every embryo has the best possible chance to grow.
The role of an embryologist goes far beyond science. They not only handle delicate laboratory work but also ensure that embryos develop under stable conditions, sometimes using advanced technology such as time-lapse monitoring or artificial intelligence. Their contribution is vital for fertility treatments everywhere, because without their careful attention, the IVF process could not succeed.
In this article, we will look at the journey from egg retrieval to embryo transfer, explore how embryos are nurtured in the IVF lab, and show why laboratory conditions are just as important as medical treatment. We will also explain how genetic testing and AI support embryo selection, and why patient communication is an essential part of an embryologist’s daily work. By the end, you will understand how embryologists combine technical expertise with emotional resilience to help many patients on their IVF journey and achieve their dream of parenthood.
Embryologist
An embryologist is at the heart of the IVF lab, guiding the earliest stages of life with precision and care. While doctors prescribe medication and perform procedures, it is the embryologists who make sure that eggs and sperm are handled correctly, fertilisation is confirmed, and embryos develop in the safest possible way. The role of an embryologist is often hidden from patients, yet they play a vital role in every IVF cycle. Without their expertise, the process of in vitro fertilisation could not succeed.
The role of an embryologist in fertility treatment
Embryologists work closely with doctors and nurses but focus on the laboratory side of infertility treatment. Their tasks range from preparing eggs after retrieval to selecting sperm and guiding fertilisation, to watching embryos grow day by day in the incubator. A skilled embryologist combines a strong scientific background with practical experience, and their work requires both technical skill and emotional strength. Every embryo represents a family’s hope, and that gives each step great responsibility.
Why embryologists play a vital role in every IVF cycle
The work of embryologists is not limited to routine tasks. It is about constant attention to detail and continuous learning, because the field of embryology is always evolving. Within the fertility team, every decision can influence whether an embryo develops well enough for transfer. This is why embryologists play a vital role in achieving higher success rates – their expertise creates the foundation for everything that follows in the IVF journey.
Egg retrieval and fertilisation
Egg retrieval is one of the first big steps in an IVF cycle. On this day, eggs are collected from the ovaries and passed directly into the hands of the embryology team. Each egg is carefully identified and placed in culture dishes, ready to meet sperm in the IVF lab. This moment is often filled with hope for patients, because it marks the beginning of embryo development outside the body. For embryologists, it is the point where great responsibility begins, as every oocyte needs to be handled with care and precision.
How eggs and sperm are prepared in the IVF lab
Once egg collection is complete, embryologists examine the aspirated fluid under the microscope to find oocytes. Each egg is washed, assessed for maturity, and placed in a dish with special culture media. At the same time, sperm is prepared by removing dead cells and debris, leaving only the strongest gametes. When eggs and sperm are ready, insemination takes place. In some cases, fertilisation happens naturally in the dish, with sperm swimming towards the egg. In other cases, a single sperm is injected directly into an egg using intracytoplasmic sperm injection.
Natural fertilisation and ICSI under the microscope
The fertilization process is one of the most delicate stages of the IVF cycle. Under the microscope, embryologists check whether an egg has been fertilised – usually visible through the appearance of two pronuclei inside the cell. When ICSI is used, the process involves even more precision, as a single sperm is introduced into each mature egg. Both methods are designed to fertilize the egg and support embryo development. For many patients undergoing IVF, this is the stage where science and hope meet, as new embryos are created in the lab from the union of eggs and sperm.
“ESHRE guidelines highlight many factors in IVF, but in my eyes the experience of embryologists is what truly makes the difference. Without them, success rates would simply not be the same.”
Nathalie Wiederkehr
Embryo development
Once fertilisation has taken place, the focus shifts to embryo development. In the IVF lab, embryos are placed in culture dishes with nutritive media and stored in incubators that maintain body-like conditions. From this moment, embryologists watch as embryonic development begins, with cells dividing and growing into new structures. Each embryo represents a unique chance of pregnancy, and the way it develops over the first few days will help determine whether it can be transferred or frozen for future use.
From early cell division to the blastocyst stage
On the first day after fertilisation, embryologists look for pronuclei, which indicate that both sets of genetic material are present. Over the next few days, embryo growth continues through rapid cell division – from just a few cells to more than a hundred by day five. At this stage, the embryo becomes a blastocyst, with an inner cell mass that will form the baby and a trophectoderm that develops into the placenta. These stages are monitored daily, with careful notes on embryo culture to track progress and catch any irregularities.
How embryologists grade embryos for transfer or freezing
Not all embryos develop at the same speed or quality, which is why embryo grading is so important. Embryologists assess factors such as cell number, symmetry, and fragmentation to decide which embryos have the best potential. Some may be selected for fresh transfer, while others are preserved through cryopreservation. Embryo freezing allows patients to return later without going through another egg retrieval, and these embryos can be thawed when needed. In some cases, preimplantation genetic testing such as PGT-A is carried out by analysing a few trophectoderm cells. Although the genetic analysis is usually performed in a separate laboratory, embryologists perform the biopsy and make sure embryos remain safe. This combination of grading, freezing, and sometimes testing gives patients more options and supports better success rates.
Embryo transfer
Embryo transfer is often described as the most emotional step of the IVF journey. After days of careful observation in the lab, selected embryos are prepared to be transferred back into the uterus. For patients, this is the moment where science and hope meet, and for embryologists it is the final handover of their work. Although the procedure itself is simple and usually painless, the preparation and decision-making behind it are complex and require great responsibility.
What happens when embryos are transferred back into the uterus
The transfer usually takes place on day three or day five, depending on how embryo development has progressed. Guided by ultrasound, a thin catheter is used to place one or more embryos into the uterus. From the outside it looks straightforward, but it is the result of days of work in the IVF lab, where every embryo was carefully nurtured and graded. At this stage, implantation is out of human hands – but ensuring that the embryos are strong and ready is what makes the difference.
How embryologists support implantation chances
Embryologists help improve the chances of implantation by preparing embryos in the best possible condition before transfer. This may involve selecting the strongest blastocyst, ensuring embryos have been cultured under optimal conditions, or integrating results from treatment plans such as preimplantation genetic testing. Their work continues even after transfer, since remaining embryos can be cryopreserved for future use. For patients, knowing that embryologists have done everything possible in the lab provides reassurance during the two-week wait, one of the most challenging parts of the IVF process.
Laboratory conditions and quality control
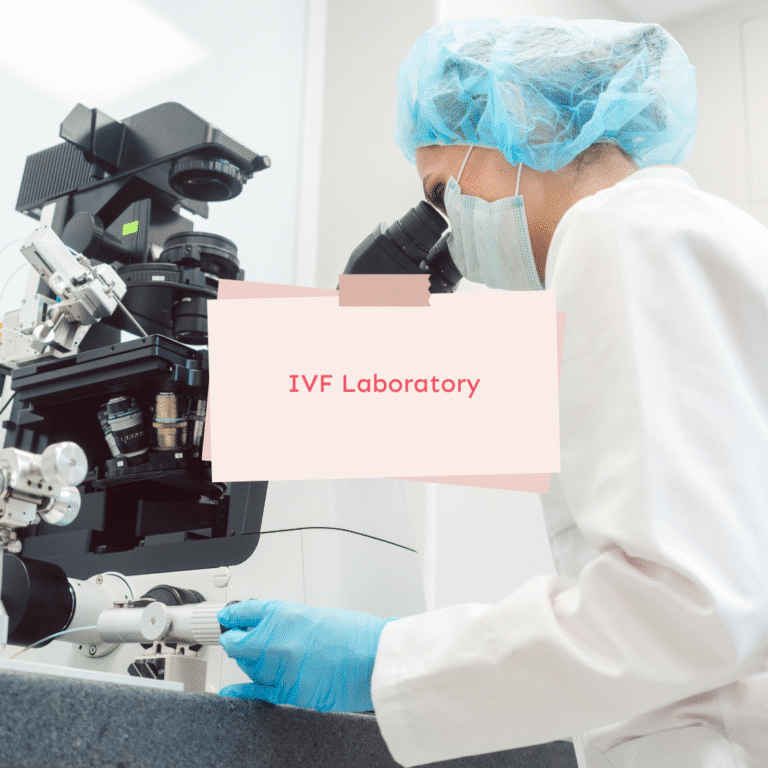
What happens inside the IVF lab is just as important as the medical procedures you see at the clinic. Embryos are extremely sensitive, and even small changes in their environment can affect embryo growth. This is why embryologists focus so much on laboratory conditions and quality control – keeping the air clean, equipment sterile, and culture systems stable. Creating optimal conditions is not a one-time effort but a continuous routine, carried out every day to give embryos the best chance of survival and development.
Why air quality, cleaning, and monitoring matter in the IVF lab
Embryos spend their earliest days in culture media, and any disturbance in air quality, temperature, or pH can interrupt embryo development. IVF labs are therefore equipped with high-grade filters, positive air pressure systems, and strict cleaning routines to minimise dust, bacteria, and chemicals. Surfaces are disinfected regularly, and the air is monitored for particles and volatile compounds that could harm embryos. Even the smallest variation can make a difference, which is why embryologists treat quality control as part of their daily responsibility. For patients, these invisible details are what contribute to higher success rates.
The role of incubators, time-lapse, and technological advancements
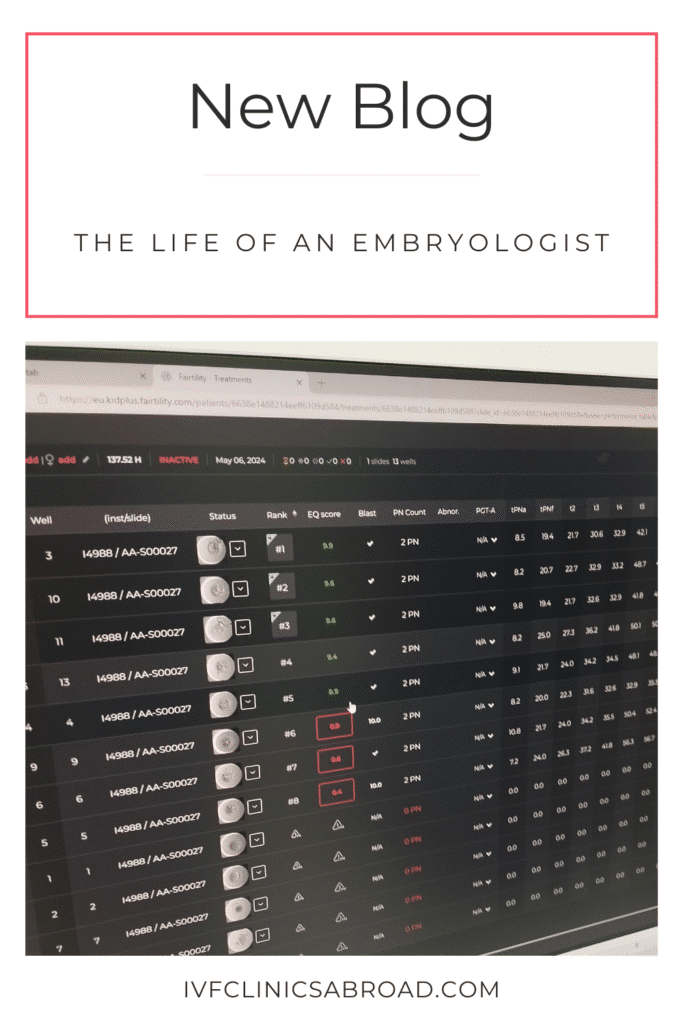
Embryos are kept in incubators that regulate temperature, humidity, and gas levels with extreme precision. In modern labs, many incubators are combined with time-lapse cameras that record the entire embryo culture without removing the embryos. This reduces stress, keeps conditions stable, and provides embryologists with thousands of images to analyse. Increasingly, AI systems are used alongside time-lapse monitoring to identify patterns in embryo development that may not be visible under the microscope. These technological advancements allow embryologists to select embryos with greater confidence, while cryopreservation techniques ensure that embryos can be safely frozen and thawed when needed. All of these measures together form the backbone of reproductive medicine, making sure embryos grow in the safest possible environment.
Genetic testing and AI
Not every embryo is genetically healthy, and one of the advances in reproductive medicine is the ability to check this before transfer. Genetic testing has become an important option in IVF, particularly for couples with a history of miscarriage or failed cycles. Today, preimplantation genetic testing (PGT) allows embryologists to identify embryos that are more likely to result in a successful pregnancy, reducing uncertainty for many patients undergoing IVF. At the same time, artificial intelligence has started to transform the way embryos are selected, adding a new layer of precision to the process.
Preimplantation testing and what it can reveal
PGT begins with a biopsy, usually taken from the trophectoderm cells of a blastocyst. These cells, which later form the placenta, can be removed without harming the embryo itself. The sample is then sent to a genetics laboratory for analysis. PGT-A can detect whether an embryo has the correct number of chromosomes, which is essential for implantation and healthy development. While embryologists do not perform the genetic analysis themselves, they play a critical role in preparing embryos, performing the biopsy, and ensuring samples remain safe. This collaboration is an important advancement in reproductive medicine and part of many treatment plans.
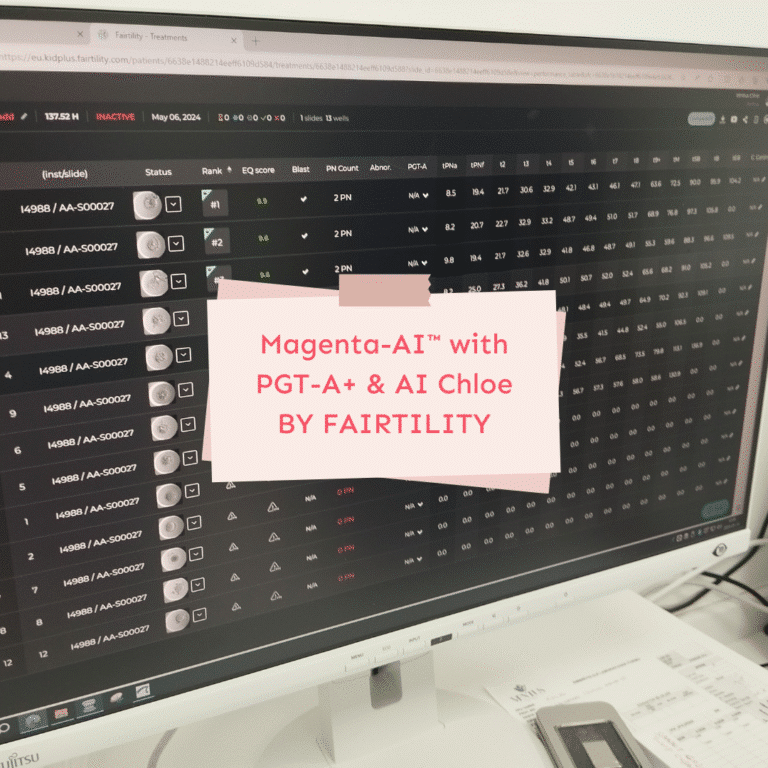
How AI is changing embryo selection and IVF outcomes
Until recently, embryo selection relied mainly on what embryologists could see under the microscope: cell number, symmetry, and fragmentation. While this method is still valuable, artificial intelligence is now providing additional insights. AI systems analyse thousands of time-lapse images of embryo development, recognising patterns invisible to the human eye. This helps predict which embryos are most likely to implant, supporting better IVF outcomes and potentially higher success rates. For patients, it means that decisions are no longer based solely on appearance but also on data-driven predictions. As the field of embryology is continuously evolving, the integration of AI marks one of the most promising technological advancements, combining human expertise with machine learning to help people achieve their dream of parenthood.
Interactions with patients
Although embryologists spend much of their time in the laboratory, patient contact is also part of their daily work. For many patients undergoing IVF, updates about embryo development are some of the most anticipated moments of the treatment. Embryologists are often the ones who explain how fertilisation went, how many embryos have developed, or whether embryo freezing is an option. These conversations carry significant emotional weight, because they connect laboratory results directly to the hopes and expectations of patients.
Communicating results and guiding treatment plans
When embryos are fertilised or transferred, embryologists often speak with patients to share results and discuss treatment plans. They may explain how many eggs were retrieved, how many embryos fertilised successfully, or what the next steps might be. For many patients, this is the first time they hear scientific details explained in simple terms. Clear communication helps reduce anxiety and builds trust, showing patients that their embryos are being cared for with precision and compassion.
Balancing technical aspects with emotional resilience
Every update an embryologist gives is more than just a number or result – it is a message that can bring relief, hope, or sometimes disappointment. This requires emotional resilience and emotional strength, as embryologists must balance the technical aspects of their work with empathy for patients. Their role is not only to support embryo development in the lab but also to reassure families that every possible step is being taken. In this way, embryologists contribute not only to the science of IVF but also to helping people achieve their dream of parenthood.
Life of an embryologist
The life of an embryologist is a mix of technical expertise, quiet dedication, and deep emotional responsibility. Most of the work happens behind closed doors in the IVF lab, yet every step connects directly to the hopes of patients trying to conceive. Embryologists work with embryos at their most fragile stage, and their decisions can influence whether a new life has the chance to grow. This profession requires not only a strong foundation in biology but also emotional strength, because the outcome of each IVF cycle is so personal for many patients.
A day in the lab and the responsibilities it includes
A typical day in the life of an embryologist includes preparing dishes for insemination, checking fertilisation results under the microscope, grading embryos, and managing cryopreservation. The responsibilities of an embryologist include maintaining incubators, monitoring air quality, and recording every technical detail with accuracy. This role carries great responsibility because a single oversight could affect embryo development. Continuous learning is part of the profession, since the field of embryology is constantly evolving with technological advancements such as time-lapse imaging and AI systems.
The challenges and rewards of helping people achieve parenthood
While the technical aspects of embryology can be demanding, the emotional side is just as powerful. Embryologists balance challenges like long hours and high concentration with the rewards of seeing embryos develop into healthy pregnancies. Many describe it as a career that constantly reminds them of the dream of parenthood they are helping others achieve. The path to becoming an embryologist usually involves a degree in biology or a related field, sometimes followed by specialised training in embryology, reproductive biology, or biomedical science. It is a career where knowledge and compassion meet, and where the challenges are outweighed by the rewards of helping families grow.
Why embryologists are the heart of reproductive medicine
Working as an embryologist means carrying both scientific and emotional responsibility. From egg retrieval to embryo transfer, from maintaining laboratory quality to guiding patients with care, their work forms the foundation of every IVF cycle. The role of an embryologist is constantly evolving, shaped by technological advancements like AI and genetic testing, yet it always comes back to one goal – helping people achieve their dream of parenthood.
If you are considering IVF abroad, it can feel overwhelming to understand which countries offer which possibilities. That is why we created a guide to IVF treatments in Europe. It explains where options such as gender selection, egg donation, or embryo donation are available, and includes an example of a clinic in Northern Cyprus with prices and success rates.
Your IVF journey is unique, and choosing the right destination is just as important as understanding the science. If you would like personal support in exploring your options, you are welcome to reach out for a private consultation.
PS: This article was written by an embryologist from Palestine, sharing her professional experience inside the IVF laboratory.