Gender Selection
Gender selection is a topic that often comes up long before clear information does. Many people encounter strong opinions, promises, or simplified explanations, while the medical reality is rarely explained in a calm and structured way. This makes it difficult to understand what gender selection can actually do and where its limits clearly are.
On this page, we explain gender selection as it is used in reproductive medicine today. We look at how it works, which methods are considered reliable, and what matters in practice when people explore this option. The goal is not to convince you of anything, but to give you a clear and realistic overview, so you can understand the topic without pressure or exaggeration.
What is gender selection
Gender selection refers to identifying the biological sex of an embryo before pregnancy begins. This is only possible through medical procedures that take place during fertility treatment. Gender selection does not influence fertilisation itself and does not change the genetics of an embryo. It simply makes existing genetic information visible.
Definition of gender selection in reproductive medicine
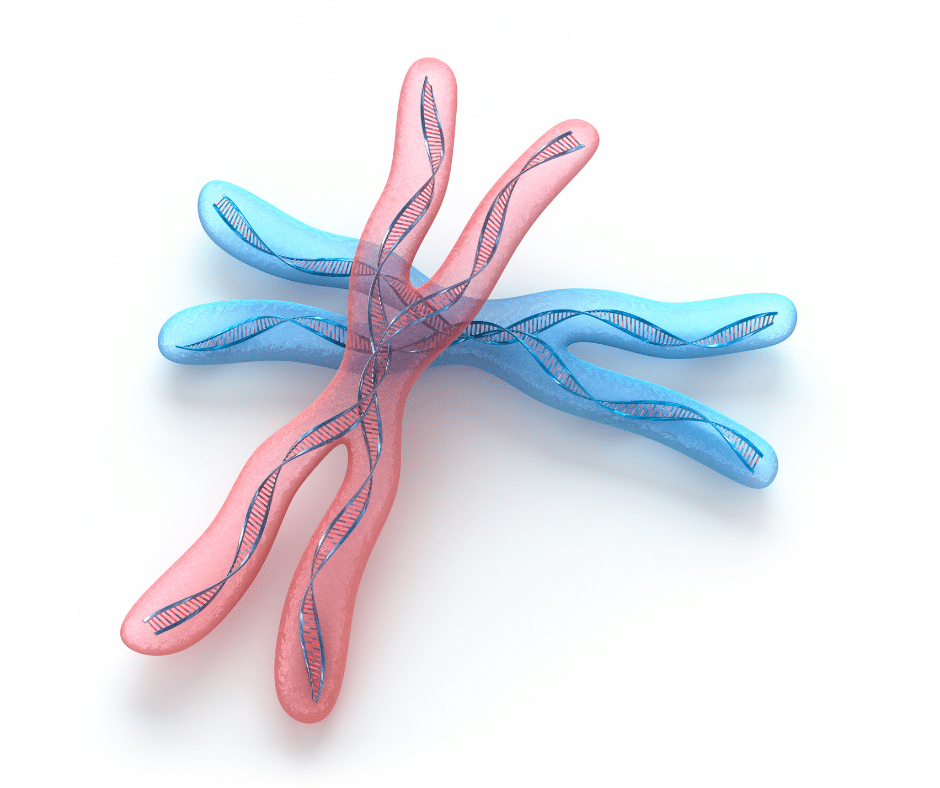
In reproductive medicine, gender selection means determining whether an embryo has two X chromosomes or one X and one Y chromosome. This information becomes available through genetic testing of embryos that have already been created in the laboratory. Based on these results, embryos of a specific sex can be selected for transfer.
Gender selection is not a treatment on its own. It is always part of a broader fertility process and depends on the creation of embryos in the first place. If no embryos develop, or if embryos are not suitable for testing, gender selection is not possible. This is an important point that is often overlooked in simplified explanations.
Basic principles of gender selection
The biological sex of an embryo is defined at the moment egg and sperm come together. From that point on, the chromosomal structure is fixed. Gender selection does not alter this structure. It only identifies it through genetic analysis.
Because this analysis takes place in the laboratory, gender selection is limited to situations where embryos exist outside the body for a short time. Natural conception, timing methods, or lifestyle changes cannot reliably determine or influence chromosomal sex. Medical gender selection is therefore based on diagnosis and selection, not influence or prediction.
How gender selection works
To understand how gender selection works, it helps to look at what determines biological sex and at which point this information becomes accessible during fertility treatment.
Role of chromosomes in gender determination
Every embryo has a fixed chromosomal makeup from the moment fertilisation happens. One pair of chromosomes determines biological sex. Embryos with two X chromosomes will develop as female, while embryos with one X and one Y chromosome will develop as male. This combination is set at fertilisation and cannot be changed later.
During fertility treatment, embryos are allowed to develop in the laboratory for several days. At a specific stage, a small number of cells can be analysed. This analysis makes it possible to see which chromosomes are present, including the sex chromosomes. Gender selection is therefore based on identifying existing genetic information, not on influencing or modifying it.
Difference between natural conception and gender selection with IVF
With natural conception, there is no medical access to embryos before pregnancy begins. The chromosomal sex remains unknown until later in pregnancy, and there is no reliable way to influence the outcome beforehand. Timing methods, diets, or lifestyle recommendations do not change chromosomal results.
With fertility treatment, embryos exist outside the body for a short time. This allows genetic testing to take place before implantation. Gender selection becomes possible only because embryos can be examined at this stage. Without laboratory access to embryos, reliable gender selection cannot occur. This difference explains why medical gender selection is limited to fertility treatment and cannot be replicated naturally.
Methods of gender selection

Natural gender selection methods and limitations
Natural gender selection methods are usually based on timing, diet, or lifestyle recommendations. Popular examples include specific intercourse timing, dietary changes, or traditional prediction tools. These approaches are widely shared because they are simple and do not require medical treatment.
What they all have in common is that they do not provide reliable control over chromosomal sex. At best, outcomes are coincidental. There is no scientific evidence showing that natural methods can consistently influence whether an embryo develops as male or female. For this reason, natural approaches are not considered gender selection in a medical sense.
Laboratory based gender selection techniques
Laboratory based methods aim to work with sperm or embryos under controlled conditions. One approach that is sometimes mentioned is sperm sorting, where sperm cells are separated based on physical characteristics. While this can slightly influence probability in certain cases, it does not offer certainty and does not involve analysing embryos themselves.
Because sperm sorting does not confirm the chromosomal makeup of an embryo, it is considered limited. It may change odds marginally, but it cannot guarantee results. For people who need clarity or have medical reasons, this level of uncertainty is often not sufficient.
Gender selection with IVF and genetic testing
The only method that allows reliable gender selection is genetic testing of embryos created during fertility treatment. Once embryos have developed in the laboratory, a small number of cells can be analysed to determine their chromosomal structure. This includes identifying the sex chromosomes.
This approach does not increase the chance of pregnancy. It provides information that allows selection among existing embryos. It simply provides information that allows selection among existing embryos. Because of this, gender selection through fertility treatment is based on diagnosis and choice, not influence or prediction.
Preimplantation genetic testing and gender selection
Preimplantation genetic testing is not performed to change embryos. It is used to analyse embryos that already exist, so informed decisions can be made before a transfer takes place.
PGT-A and gender selection
PGT-A is a form of genetic testing that looks at the number of chromosomes in an embryo. One part of this analysis includes the sex chromosomes. This means that, alongside information about chromosomal balance, the biological sex of an embryo becomes visible.
In practice, PGT-A is often used to reduce the risk of transferring embryos with chromosomal abnormalities. Gender selection is therefore usually a secondary result of this testing, not its primary medical purpose. This distinction matters, because it explains why gender selection is always tied to a broader fertility process and not offered as an isolated procedure.
Difference between PGT-A PGT-M and PGT-SR
There are different types of preimplantation genetic testing, each with a specific focus. PGT-A looks at chromosome number, PGT-M targets specific inherited conditions, and PGT-SR focuses on structural chromosomal rearrangements.
When people talk about gender selection, they often use these terms interchangeably, even though they serve different purposes. What they have in common is that they analyse embryos at an early stage. Gender information becomes available because sex chromosomes are part of the genetic data, not because the test was designed to select gender alone.
Embryo biopsy and genetic analysis
Genetic testing requires a biopsy, meaning that a small number of cells are taken from an embryo at a defined stage of development. This process is carefully controlled and performed by experienced laboratories. The embryo itself is not altered, and testing focuses on analysing the cells that are removed.
Results from genetic analysis provide information about chromosomal structure, including sex chromosomes. Only after these results are available can decisions about embryo transfer be made. This step explains why gender selection is dependent on laboratory quality, experience, and clear communication about what the test can and cannot show.
Gender selection success rates

Accuracy of gender selection
When genetic testing is used, the chromosomal sex of an embryo can be identified with a very high level of accuracy. Because the analysis looks directly at the sex chromosomes, the result is considered reliable. Errors are rare and usually related to technical issues rather than biological uncertainty.
This means that when an embryo is identified as male or female through genetic testing, the information itself is dependable. Gender selection, in this sense, is not a matter of probability or estimation. It is based on analysing existing genetic data.
IVF success rates versus gender selection accuracy
Accurate gender identification does not automatically mean a successful pregnancy. Even if the chromosomal sex is known with certainty, implantation and pregnancy depend on many other factors. Embryo quality, uterine conditions, age, and overall fertility history all play a role.
This distinction is important because it explains why gender selection does not guarantee a live birth. Selecting the sex of an embryo does not change its ability to implant or develop. Gender selection provides information, but it does not improve or reduce the inherent chances of pregnancy.
Factors influencing outcomes
The number of embryos available is one of the most relevant factors. Not every fertility cycle results in multiple embryos, and not every embryo is suitable for testing or transfer. In some cases, embryos of the desired sex may not be available at all.
Laboratory experience, testing methods, and overall treatment planning also influence outcomes. This is why gender selection is always discussed within the broader context of fertility treatment, rather than as a standalone option. Understanding these limitations early helps avoid expectations that cannot be met.
Legal aspects of gender selection
Questions about legality often come up early, and for good reason. Gender selection is not regulated in the same way everywhere, and the legal framework can feel confusing at first glance. What matters in practice is understanding how different countries approach the topic and why these differences exist.
Medical and non-medical gender selection
In many countries, gender selection is legally permitted only when there is a medical reason, such as reducing the risk of passing on a serious genetic condition. In these cases, gender selection is seen as part of preventive medical care rather than a personal choice.
Non-medical gender selection, often discussed in the context of family balancing, is treated more restrictively. Some countries explicitly prohibit it, others do not clearly regulate it. This distinction explains why access to gender selection depends not only on medical technology, but also on how laws define acceptable use.
Gender selection laws in different countries
Legal approaches to gender selection vary widely. Some countries have clear regulations that outline when and how gender selection is allowed. Others operate in a more ambiguous legal environment, where the procedure is technically possible but not openly addressed in legislation.
Because of these differences, many people consider treatment abroad. The decision is often less about avoiding rules and more about seeking clarity, transparency, and predictable processes. Understanding the legal context of the country where treatment takes place is an essential part of planning.
Disclosure of embryo gender
Even when genetic testing is permitted, laws may restrict what information clinics are allowed to share. In some countries, clinics may perform genetic testing but are not allowed to disclose the sex of the embryo unless there is a medical indication.
This means that access to gender information does not always depend on whether testing is possible, but on whether disclosure is allowed. This detail is frequently overlooked and can lead to misunderstandings if it is not clarified in advance.

Costs of gender selection
Factors influencing gender selection costs
The cost of gender selection is influenced by several components. Fertility treatment itself, laboratory procedures, and genetic testing are usually calculated separately. The type of genetic test used, the number of embryos analysed, and the technology available in the laboratory all play a role.
Medication, monitoring, and the number of treatment cycles needed also affect the total cost. Because not every cycle results in embryos suitable for testing, costs can vary even for people following a similar treatment path.
Differences between countries and clinics
Treatment costs differ widely between countries. This is partly due to healthcare systems, regulatory requirements, and operating costs. In some regions, fertility treatment is highly standardised and expensive. In others, clinics operate with lower overheads and offer more flexible pricing models.
Clinics may also differ in what they include in their packages. Some quote a basic price and add costs later, while others offer more comprehensive pricing from the start. This makes direct comparisons difficult unless the details are carefully reviewed.
Genetic testing costs
Genetic testing itself can vary in scope and price. Some tests analyse only selected chromosomes, while others provide a full chromosomal overview. More extensive testing usually comes with higher costs, but it also provides more information.
Understanding what kind of testing is included helps avoid misunderstandings later. The lowest price is not always the most informative option, and higher costs do not automatically mean better outcomes. What matters is whether the testing approach matches the individual situation and expectations.
Choosing a clinic for gender selection
Choosing a clinic is not just about success rates or technology. It is about clarity, experience, and how openly information is shared. Gender selection requires precise laboratory work and clear communication, which makes the choice of clinic especially relevant.
Experience with genetic testing
Not every fertility clinic has the same level of experience with genetic testing. Some clinics work with these methods on a daily basis, others only occasionally. Experience matters because genetic testing and embryo handling require well-established routines and close coordination between medical and laboratory teams.
Clinics that regularly work with genetic testing are usually clearer about what is possible and what is not. They are also better prepared to explain results in a way that makes sense without overpromising outcomes.
Laboratory standards and transparency
Laboratory quality plays a central role in gender selection. This includes how embryos are cultured, how biopsies are performed, and how genetic analysis is handled. While these details are rarely visible from the outside, they directly influence reliability and communication.
Transparency is just as important as technical standards. Clinics should be able to explain which tests they use, how results are reported, and what happens if outcomes differ from expectations. Clear answers at this stage help avoid misunderstandings later in the process.

How gender selection works
To understand how gender selection works, it helps to look at what determines biological sex and at which point this information becomes accessible during fertility treatment.
Role of chromosomes in gender determination
Every embryo has a fixed chromosomal makeup from the moment fertilisation happens. One pair of chromosomes determines biological sex. Embryos with two X chromosomes will develop as female, while embryos with one X and one Y chromosome will develop as male. This combination is set at fertilisation and cannot be changed later.
During fertility treatment, embryos are allowed to develop in the laboratory for several days. At a specific stage, a small number of cells can be analysed. This analysis makes it possible to see which chromosomes are present, including the sex chromosomes. Gender selection is therefore based on identifying existing genetic information, not on influencing or modifying it.
Difference between natural conception and gender selection with IVF
With natural conception, there is no medical access to embryos before pregnancy begins. The chromosomal sex remains unknown until later in pregnancy, and there is no reliable way to influence the outcome beforehand. Timing methods, diets, or lifestyle recommendations do not change chromosomal results.
With fertility treatment, embryos exist outside the body for a short time. This allows genetic testing to take place before implantation. Gender selection becomes possible only because embryos can be examined at this stage. Without laboratory access to embryos, reliable gender selection cannot occur. This difference explains why medical gender selection is limited to fertility treatment and cannot be replicated naturally.
Methods of gender selection

Natural gender selection methods and limitations
Natural gender selection methods are usually based on timing, diet, or lifestyle recommendations. Popular examples include specific intercourse timing, dietary changes, or traditional prediction tools. These approaches are widely shared because they are simple and do not require medical treatment.
What they all have in common is that they do not provide reliable control over chromosomal sex. At best, outcomes are coincidental. There is no scientific evidence showing that natural methods can consistently influence whether an embryo develops as male or female. For this reason, natural approaches are not considered gender selection in a medical sense.
Laboratory based gender selection techniques
Laboratory based methods aim to work with sperm or embryos under controlled conditions. One approach that is sometimes mentioned is sperm sorting, where sperm cells are separated based on physical characteristics. While this can slightly influence probability in certain cases, it does not offer certainty and does not involve analysing embryos themselves.
Because sperm sorting does not confirm the chromosomal makeup of an embryo, it is considered limited. It may change odds marginally, but it cannot guarantee results. For people who need clarity or have medical reasons, this level of uncertainty is often not sufficient.
Gender selection with IVF and genetic testing
The only method that allows reliable gender selection is genetic testing of embryos created during fertility treatment. Once embryos have developed in the laboratory, a small number of cells can be analysed to determine their chromosomal structure. This includes identifying the sex chromosomes.
This approach does not increase the chance of pregnancy. It provides information that allows selection among existing embryos. It simply provides information that allows selection among existing embryos. Because of this, gender selection through fertility treatment is based on diagnosis and choice, not influence or prediction.

Practical aspects of gender selection
Treatment planning and timelines
Gender selection is not a one-day decision or a single appointment. It is part of a fertility treatment process that unfolds over several stages. Preparation, stimulation, egg retrieval, laboratory development, genetic testing, and embryo transfer all follow a defined sequence.
The overall timeline depends on individual circumstances and on whether treatment is done in one cycle or spread over several steps. Some clinics work with fresh transfers, others with frozen embryos after testing. Understanding the timeline early helps set realistic expectations and makes planning easier, especially when work or family commitments are involved.
Travel and discretion
Many people who consider gender selection travel abroad for treatment. Travel usually involves staying near the clinic for a limited period, rather than relocating for weeks. The length of stay depends on the treatment phase and the clinic’s protocol.
Discretion is a common concern. Some prefer to keep treatment private, others want to minimise questions from their surroundings. Clinics that regularly work with international patients are usually familiar with these concerns and can help structure appointments and communication accordingly. Knowing what support is available makes the practical side feel more manageable.
Who gender selection may be suitable for

Medical and personal considerations
In some cases, gender selection is considered because of medical reasons, such as the risk of passing on a sex-linked genetic condition. In other situations, the motivation is personal, often connected to family balancing or long-term wishes about family structure.
What matters is understanding that gender selection does not replace fertility treatment and does not change underlying fertility factors. For people with a low ovarian reserve or repeated treatment failures, expectations may need to be adjusted early.
Emotional readiness and expectations
Gender selection can create very specific expectations. While knowing the chromosomal sex of an embryo provides clarity, it does not remove uncertainty around implantation or pregnancy. Being prepared for this distinction helps avoid disappointment later.
It is also important to feel comfortable with the process itself. Gender selection involves testing, waiting for results, and making decisions based on probabilities and availability. For some, this feels empowering. For others, it adds pressure. Understanding your own limits is part of deciding whether this path is suitable.
Ethical considerations around gender selection
Why gender selection raises ethical questions
Gender selection touches on questions about choice, responsibility, and how medical technology is used. Some concerns focus on whether selecting the sex of an embryo could reinforce social preferences or inequalities. Others relate to how far medical intervention should go when it comes to reproduction.
These questions do not have simple answers. Ethical concerns are shaped by cultural values, historical context, and individual experiences. This is one reason why laws and medical guidelines differ so widely between countries.
Personal decision making and ethical boundaries
For many people, the ethical aspect of gender selection is deeply personal. Some feel comfortable with the idea, especially when medical reasons are involved. Others draw clear boundaries based on personal values or beliefs.
What matters in practice is being aware of these questions and taking time to reflect on them. Gender selection is not just a technical process. It is a decision that sits at the intersection of medicine, personal values, and societal norms. Approaching it with awareness rather than certainty allows for more grounded decision making.
Next steps after learning about gender selection
After learning how gender selection works, many people feel clearer, but not necessarily ready to decide. This is normal. Gender selection involves medical, practical, and personal considerations, and there is no need to move faster than feels right.
A useful next step is often to look at how gender selection is approached in different countries. Legal frameworks, costs, and reported success rates vary, and general explanations rarely show how these differences play out in practice. Seeing concrete examples can help put information into context without turning it into a decision.
For this reason, we have put together a guide that outlines where gender selection is possible and how legal access, pricing, and success rates can differ between countries. The guide is meant as an orientation tool, not a recommendation, and focuses on helping you understand the landscape before taking any further steps.
Some prefer to continue researching independently, while others find it helpful to compare information with clearer reference points. What matters is choosing a pace and level of detail that supports clarity rather than pressure.
