How next-generation sequencing (NGS) is used in IVF for embryo testing and better outcomes
IVF: Genetic Testing with Next Generation Sequencing (NGS). Improve IVF success with NGS embryo screening. Advanced reproductive medicine, genetic sequence analysis.
If you’re thinking about IVF and wondering how to improve your chances, you’re not alone. Many women ask themselves: is there a way to reduce the risk of miscarriage, or to avoid passing on a genetic condition? One method that can help is called next generation sequencing – or NGS.
NGS is a genetic test that looks closely at the DNA of each embryo. It helps identify which embryos are most likely to develop into a healthy pregnancy. This means fewer uncertainties, and sometimes fewer failed attempts.
To do this, a few cells are taken from each embryo and analysed in a lab. Specialists look at the DNA sequence and check for abnormalities. Only embryos with a normal genetic profile are selected for transfer.
NGS is more detailed than older methods. It gives doctors a clearer view of the embryo’s genetic health. That makes planning more precise – especially when there’s a known risk in the family.
But the process takes time. The embryos are frozen while the lab works on the analysis. You usually need to travel again for the transfer, once the results are ready. So it’s not suitable for every situation.
Still, for many women, it’s a helpful step. If you’re looking for clarity, NGS might give you just that. In this guide, we’ll walk you through how it works and what to expect – gently, and one step at a time.
What is next generation sequencing technologies (NGS) and how does it work?
Next generation sequencing, often called NGS, is a genetic testing method. It is used to examine the DNA of embryos before they are transferred during IVF. The goal is simple: to find embryos with normal genetic makeup.
During the test, specialists take a few cells from each embryo. These cells are then sent to a lab, where the DNA is carefully analysed. The process involves reading the DNA step by step, like decoding a very long instruction manual.
With NGS, it’s possible to spot problems in the embryo’s chromosomes. These problems might lead to miscarriage or genetic diseases later on. By checking this in advance, clinics can select embryos that are more likely to grow into a healthy pregnancy.
The method is more advanced than older techniques. It gives a deeper and more detailed view of the embryo’s genetic health. This is why more clinics now use NGS as part of the IVF process – especially in complex cases or when someone has had repeated failed treatments.
NGS is not a guarantee. But it offers an extra layer of insight. For many women and couples, that insight is a huge step towards clarity, trust and better planning.
Understanding genetic problems in fertility with pre-implantation genetic testing
Not every difficulty with getting pregnant has a clear explanation. Sometimes, it’s simply timing or stress. But in other cases, a hidden genetic issue might be the reason why things aren’t working out.
Genetic problems can affect both women and men. Sometimes, one partner carries a change in their DNA that doesn’t cause symptoms but still gets passed on. This can lead to embryos with missing or extra chromosomes. In many cases, these embryos stop developing naturally – often before a woman even knows she was pregnant.
This is one reason why miscarriages happen, especially early on. And in IVF, it’s also why not every embryo leads to a successful pregnancy, even if it looks perfect under the microscope.
Genetic conditions don’t always run in the family. They can appear by chance, especially as we get older. That’s why women over 35 are often offered genetic testing as part of their fertility journey. It’s not about fear – it’s about having more information.
By understanding these possible problems, it becomes easier to make decisions. Whether you’re trying naturally or planning IVF, knowing what’s going on at the DNA level can change everything.
How NGS is used in reproductive medicine
In fertility care, next generation sequencing is used to check the genetic health of embryos before transfer. The goal is to find out which embryo has the best chance of leading to a healthy pregnancy.
This is usually done on day five of embryo development. A few cells are taken from the outer layer of the embryo, which later forms the placenta. The embryo itself is not harmed. These cells are then analysed in a lab.
NGS helps detect changes in the number or structure of chromosomes. For example, if an embryo has an extra chromosome, it might lead to miscarriage or a genetic condition. With this information, doctors can choose embryos that are most likely to implant and grow normally.
This approach is often used when there is a known risk, such as a history of miscarriage or a genetic condition in the family. But more and more clinics also use NGS routinely for women over 35 or in cases where previous IVF attempts were not successful.
The use of NGS doesn’t replace medical care or lifestyle factors. But it adds another layer of insight that can help doctors and patients make more informed choices.
Why more couples are turning to NGS for fertility treatment
More and more couples choose to include NGS in their IVF journey. One reason is the desire for clarity. When you’ve been through failed cycles or early losses, it helps to understand what might be happening at a deeper level.
NGS offers that. It doesn’t guarantee success, but it reduces uncertainty. For many, this makes the emotional part of IVF a little easier to handle.
There’s also the question of time. IVF is demanding – physically, emotionally and financially. If you only have a limited number of embryos, it makes sense to use the one with the best chance. NGS helps identify that embryo before transfer.
In some cases, couples turn to NGS because of a known genetic condition. Others choose it simply because they want to lower the risk of miscarriage. And for women over 35, where chromosomal issues become more common, it’s often recommended as part of the process.
NGS is also becoming more available. Clinics have better technology now, and the costs have gone down in many countries. That makes it easier to access for those who want this option.
For all these reasons, NGS is becoming a routine part of IVF in more and more clinics – especially when couples want to plan carefully and reduce the risk of surprises.
Increased success rates with in vitro fertilization (IVF)
NGS can help improve the chances of a successful pregnancy. By selecting embryos with the correct number of chromosomes, the risk of failure after transfer is lower. This means that each IVF cycle has a higher chance of leading to a healthy pregnancy.
Lower risk of miscarriage
One of the most difficult parts of IVF is experiencing a miscarriage after so much effort. Many miscarriages happen because of genetic problems in the embryo. With NGS, these issues can often be detected before transfer, helping to avoid this painful outcome.
Reducing the chance of genetic diseases, checking the chromosomes with genetic diagnosis
If there’s a family history of a genetic condition, NGS can be used to check whether an embryo has inherited it. This adds peace of mind for couples who want to avoid passing on a known disorder. Even in cases without a known risk, NGS can help reduce the chance of serious abnormalities.
Better planning and preparation
NGS provides information early in the process. This makes it easier to plan ahead – emotionally, medically and financially. For couples who live abroad or have limited time, it also helps coordinate treatment more clearly. Knowing which embryos are viable allows for more focused and confident decisions.
Advances in technology and accessibility
NGS has become faster, more accurate, and more affordable over the years. What was once a complex test used only in rare cases is now available in many IVF clinics. New lab equipment and better data systems have made it easier to process results quickly and reliably. As technology improves, more couples can benefit from it without long waiting times or extreme costs.
Advantages of next-generation sequencing (NGS) compared to other genetic tests
Not all genetic tests are the same. Some older methods check only a few chromosomes or focus on limited parts of the DNA. NGS offers a more detailed and modern approach. It’s not just about finding big problems – it can also detect smaller issues that might affect implantation or development.
Because of this, many clinics now prefer NGS over traditional methods. It offers a wider view, delivers more reliable results, and supports better decisions during IVF. Below are some of the main advantages that explain why NGS is becoming the standard in many fertility centres.
Higher resolution and precision
NGS looks at the embryo’s DNA in much more detail than older methods. This makes it possible to spot small changes that might be missed with standard tests. The results are more precise, which helps doctors make better decisions.
More comprehensive genome coverage
Instead of checking only a few chromosomes, NGS examines the full set. This means it can detect a wider range of potential issues, giving a more complete picture of each embryo’s genetic health.
Multiple uses beyond fertility
While NGS is mainly used in IVF to select embryos, it can also help identify inherited conditions in the parents. In some cases, it supports other medical decisions, especially if there’s a known family history.
Faster results and fewer delays
Modern labs can now process NGS results in just a few days. That means less waiting and less uncertainty. Although the embryos are usually frozen while waiting, the timing is more predictable than it used to be.
Lower costs in recent years
NGS used to be a very expensive test. But today, prices have gone down in many countries. As more clinics offer the service, it’s becoming more affordable and realistic for couples who want this option.
Are there any disadvantages or limitations?
While NGS offers many benefits, it’s not the perfect solution for everyone. Like any medical tool, it has its limits. It can bring clarity, but it also brings questions – especially when results are unclear or hard to interpret. And in some cases, the process can feel more complex than expected.
Before deciding to use NGS, it helps to understand what it can and cannot do. The following points show where limitations may appear, so you can make an informed decision.
Complex procedure and interpretation
NGS involves advanced lab work and careful timing. It also requires experienced staff to read and explain the results correctly. For patients, the steps may not feel complicated – but behind the scenes, it’s a detailed process.
Risk of errors or inconclusive results
Even with the best technology, there is always a small chance that the results may be unclear. Sometimes, cells don’t grow well in the lab. In other cases, the test can’t give a clear answer. This may delay the transfer or lead to uncertainty.
Limited ability to detect all abnormalities
NGS looks at chromosomes and many genetic patterns – but not all. Some rare or very small changes can still go unnoticed. No test can offer 100% certainty, so it’s important to know what the limits are.
Ethical concerns in embryo selection
Some people feel uneasy about selecting embryos based on their genetic profile. In some countries, there are rules about what can and cannot be tested. This raises ethical questions, especially when it comes to non-medical choices like sex selection.
High dependence on advanced data analysis
The results of NGS depend on the quality of the lab and the software used. The better the data analysis, the more reliable the outcome. But this also means that not all clinics offer the same level of accuracy. It’s important to ask how and where the test is performed.
“NGS doesn’t change the embryo – but it changes how we see it, and that changes everything.”
Nathalie Wiederkehr
How does NGS treatment actually work?
NGS is not a separate treatment. It’s part of the IVF process. The test itself happens between fertilisation and embryo transfer, but planning begins much earlier. Understanding how it fits into the overall journey helps reduce stress and avoid surprises.
From the first consultation to the embryo transfer, each step is carefully timed. Below, you’ll see how NGS is typically used during an IVF cycle.
Counselling and decision-making process
Before anything begins, you’ll talk to your doctor or a genetic specialist. They’ll explain what NGS can show and where its limits are. If you or your partner carry known genetic risks, this is the moment to discuss them. The goal is to decide together whether NGS makes sense in your case.
Genetic testing for both partners
In some clinics, both partners may be offered basic or comprehensive genetic screening. This checks whether you carry conditions that could affect the embryo. If something is found, it doesn’t mean you can’t continue – it just helps guide the use of NGS in the next steps.
Hormonal stimulation and egg collection
Like in any IVF cycle, the ovaries are stimulated with hormones to grow multiple eggs. When the eggs are ready, they are collected through a minor procedure. This is done under light sedation and usually takes less than 30 minutes.
Fertilisation and embryo development
The collected eggs are fertilised with sperm from your partner or a donor. The embryos are then cultured in the lab. On day five, when the embryos reach the blastocyst stage, a small number of cells are taken for testing.
Biopsy and DNA sequencing
A few cells are gently removed from each embryo. These cells are then frozen and sent to a genetics lab. The embryo itself is also frozen after the biopsy, so there is no fresh transfer at this stage.
Embryo freezing and delayed transfer
Because results take several days, the transfer must wait. Once the analysis is complete, the clinic will tell you which embryos are genetically normal. You can then prepare for a frozen embryo transfer in a later cycle.
Selection of embryos for transfer
Based on the results, the doctor selects one embryo for transfer – usually the one with the best genetic and visual quality. If there are several good embryos, the rest can stay frozen for future use.
Cryotransfer and pregnancy test
The chosen embryo is thawed and transferred into the uterus during a carefully timed cycle. After about 10 to 14 days, you can take a pregnancy test. This is often the hardest part – the waiting.
Monitoring pregnancy to term
If the test is positive, your care continues as in a normal pregnancy. But knowing that your embryo passed a genetic check may give you a sense of calm and reassurance in the early weeks.
Risks and side effects of NGS in fertility treatment
NGS is generally safe, and the biopsy itself is a well-established part of modern IVF. Still, it’s important to know that every step in the process comes with a few risks. Not all of them are physical – some are emotional or related to the extra time and effort involved.
Being aware of these risks doesn’t mean you should worry. It simply means you can plan with more confidence and realistic expectations.
Miscarriage and failed implantation
NGS helps reduce the risk of miscarriage by identifying embryos with genetic problems. But even a healthy-looking embryo might not implant. No test can fully prevent a miscarriage. That’s why doctors are always careful not to promise success – even when the embryo looks perfect on paper.
Risk of multiple pregnancies
In most cases, only one embryo is transferred at a time. But if more than one is used, or if embryos split after transfer, there is a chance of twins or more. This can carry extra risks for mother and baby, and needs to be discussed in advance.
Infections and complications
The egg collection and embryo transfer are minor procedures, but they still involve medical intervention. In rare cases, infections or side effects from medication can occur. Your clinic will guide you through the risks and how they’re managed.
Emotional and ethical implications
Waiting for NGS results can be stressful. It adds extra time and a second clinic visit. Some couples also feel uncomfortable choosing between embryos based on genetics. These are emotional decisions, and it’s okay to have mixed feelings. Talking about it with someone you trust can help.
Missing or inconclusive results
Sometimes the test doesn’t give a clear answer. The lab may not be able to read the DNA properly, or the result may fall into a grey area. In that case, you’ll need to decide whether to transfer the embryo anyway or wait.
What are the costs of NGS and IVF treatment?
The cost of NGS depends on where you do your treatment and how many embryos need to be tested. It’s important to separate the different parts of the process, as NGS is only one step within a full IVF cycle.
Some clinics offer packages that include everything. Others charge separately for each part. Below, you’ll find a breakdown of the typical costs involved.
Cost of hormone stimulation
Before egg collection, hormone medication is needed to stimulate the ovaries. The price can vary depending on the country and the type of drugs used. In Europe, it often ranges from 1,000 to 2,500 euros. In the USA, it may be between 3,000 and 5,000 dollars.
IVF and embryo transfer costs
The IVF procedure includes egg collection, fertilisation, embryo culture and transfer. In Northern Cyprus, prices often start from 3,000 euros. In other European countries, it’s usually between 4,000 and 8,000 euros. In the USA, full IVF cycles can cost 10,000 to 20,000 dollars or more.
NGS analysis per embryo or batch
The cost of the genetic test depends on the number of embryos analysed. In Northern Cyprus, the starting price for NGS is around 2,500 euros. In the USA, it may range from 5,000 to 10,000 dollars. Sometimes, the price is per embryo – sometimes per batch.
Price comparison: Europe vs. USA
In general, IVF with NGS is much more affordable in Europe than in the USA. Even with travel expenses, many couples find that going abroad for treatment still costs less. Countries like Northern Cyprus, Greece, Spain and the Czech Republic are popular for this reason. The choice depends on your needs – and on what is legally allowed in each country.
What are the success rates of NGS treatment?
Success in IVF depends on many things. NGS doesn’t create better embryos, but it helps identify the ones that are most likely to result in a pregnancy. This can increase the overall success rate per transfer, especially when only one embryo is used.
It’s important to know that no method can guarantee a pregnancy. But NGS offers more information – and that often leads to better pregnancy outcomes, fewer failed attempts, and more focused decisions.
Role of maternal age
Age plays a key role in fertility. As women get older, the number of genetically healthy eggs decreases. This means fewer embryos are suitable for transfer. NGS helps identify the best ones, especially for women over 35, when the risk of chromosome issues increases.
Embryo quality and number
The more embryos you have, the more options NGS can offer. If only one or two embryos develop, NGS might not be useful. But when there are several, the test can guide the decision on which embryo to transfer first – saving time, money, and emotional energy.
Experience of the clinic and medical team
Success rates also depend on the team. A skilled lab, a careful biopsy, and accurate analysis all matter. It’s worth asking how often the clinic performs NGS and who interprets the results. The test itself is powerful – but it’s only as good as the people using it.
What studies say about euploid embryo transfers
Research shows that transferring euploid embryos – embryos with the correct number of chromosomes – leads to higher pregnancy rates. In some studies, the success rate per transfer is over 60% when a tested embryo is used. This doesn’t apply to everyone, but it gives hope to couples who want to reduce the number of cycles needed.
Ethical considerations in using NGS for family planning
Using NGS brings up personal and social questions. It’s one thing to test for serious medical issues. But what about choosing between embryos? What if the clinic can also tell you the sex of each one?
These decisions are deeply personal – and they’re not always easy. Some people feel relieved to have this information. Others feel uncomfortable making choices based on genetics. That’s why it’s important to think ahead and decide what feels right for you.
In some countries, there are clear rules about what can be tested. In others, clinics are more flexible. But ethics are not just about laws. They’re about what you believe and what you want for your future child.
Here are some of the key aspects couples should consider when using NGS in family planning.
Embryo selection and social responsibility
Choosing one embryo over another can feel like a medical decision – but it can also raise social questions. What if you choose not to transfer an embryo with a low risk for a condition that may never appear? Everyone has a different view of what’s acceptable. Talking it through with your doctor can help.
Data privacy and genetic information
Genetic testing creates sensitive data. It’s important to know how this data is stored, who can access it, and how long it is kept. Ask your clinic about data protection, especially if your treatment takes place in another country.
Access, affordability and equity
Not everyone can afford NGS. And not every clinic offers it. This creates gaps – between countries, but also between people. Some families may have options that others don’t. It’s a reality that raises questions of fairness in fertility care.
Long-term societal consequences
Some experts worry that genetic testing could one day be used for more than health – for preferences. While this is not the goal of NGS today, it’s something to be aware of. The line between medical need and personal wish isn’t always clear. That’s why it’s important to stay informed and make thoughtful choices.
Where is NGS treatment available?
Not every country allows genetic testing during IVF, and the rules vary widely. In some places, NGS is fully integrated into fertility care. In others, it’s restricted or not offered at all. That’s why many couples travel abroad to access treatments that may not be legal or available at home.
If you’re considering NGS, it’s important to check both the legal framework and the practical quality of care. Some destinations combine modern labs with experienced teams and fair prices – which can make a real difference in your journey.
Here are a few countries where NGS is commonly offered.
Spain: Modern standards and wide availability
Spain is known for its advanced fertility clinics and clear legal guidelines. NGS is widely available and often used in combination with egg donation or IVF for women over 40. Clinics in Spain are experienced, and many offer care in several languages.
Czech Republic: Affordable and growing sector
The Czech Republic has become a popular destination for fertility treatments. Prices are lower than in Western Europe, and many clinics use modern NGS platforms. It’s a good option for couples looking for solid care with manageable costs.
Greece: Experienced and cost-effective clinics
Greece offers NGS in combination with IVF, and many clinics have years of international experience. The laws allow for testing in medical cases, and the approach is usually personal and flexible. It’s also an attractive country for couples combining treatment with a short break.
Northern Cyprus: Accessible option for gender selection
Northern Cyprus is one of the few places where NGS is openly used for both medical reasons and gender selection. The legal environment is more flexible, and many clinics specialise in international care. Prices are lower than in most other countries, and waiting times are short.
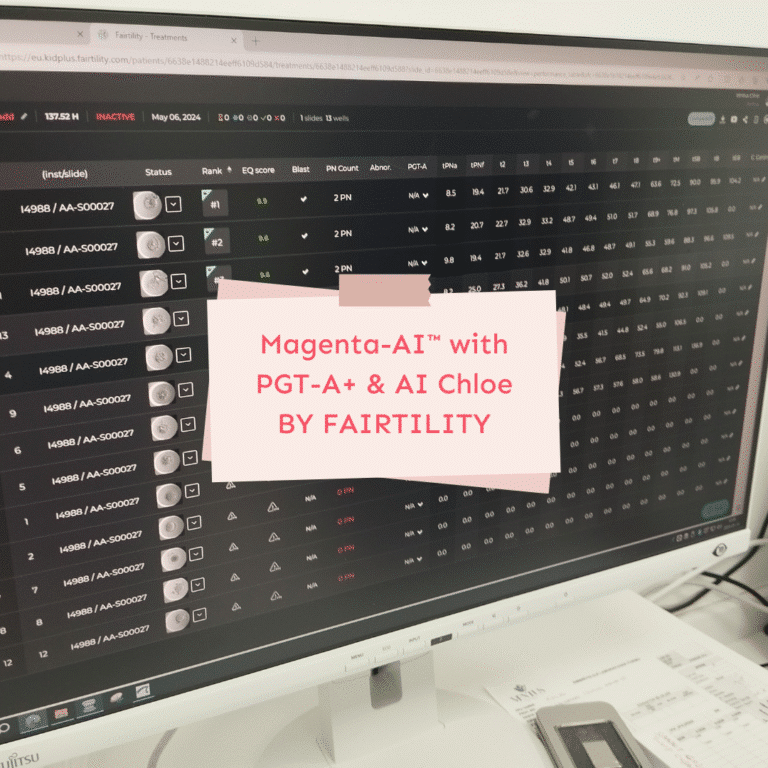
Preimplantation genetic testing for aneuploidy (PGT-A) vs. NGS: Which option is better?
When looking into genetic testing during IVF, you may come across different names. Two common terms are PGT-A and NGS. They’re often used together, but they’re not exactly the same.
PGT-A stands for preimplantation genetic testing for aneuploidy. It’s a test that checks whether an embryo has the correct number of chromosomes. NGS, or use of next-generation sequencing, is the method used to perform that test.
In simple terms: PGT-A is what you test for – and NGS is how you do it.
Older methods, like FISH, could only test a few chromosomes. NGS allows clinics to look at all chromosomes at once, in much greater detail. That’s why many clinics now use NGS to carry out PGT-A.
So it’s not really about choosing between the two. It’s about knowing how your clinic performs the test – and whether they’re using the most accurate tools available.
Here’s what you can consider when making your decision.
Differences in technique and accuracy
NGS offers higher resolution than older testing methods. It can detect small changes that other techniques might miss. If your clinic still uses older tools, ask whether they offer NGS-based testing.
Pros and cons of each method
Older methods may be faster or slightly cheaper, but they often give less information. NGS is more detailed, but it usually requires embryo freezing and a second visit for transfer. What you choose depends on what matters most to you: speed, cost, or depth of information.
Which one fits your personal situation?
Older methods may be faster or slightly cheaper, but they often give less information. NGS is more detailed, but it usually requires embryo freezing and a second visit for transfer. What you choose depends on what matters most to you: speed, cost, or depth of information.
Is NGS the right choice for you?
NGS is a powerful tool, but it’s not for everyone. Whether it makes sense in your situation depends on many things: your medical history, your age, the number of embryos, and how you feel about genetic testing in general.
Some women want as much clarity as possible. Others prefer a simpler path. Both approaches are valid. The most important thing is that your decision feels right for you.
NGS may bring peace of mind – but it also adds time, cost and a second step in the process. Knowing the benefits and limits in advance can help you feel more in control.
When to consider NGS
NGS is often helpful if you’ve had miscarriages, failed IVF cycles, or if you’re over 35. It’s also worth considering if you carry a known genetic condition. In these cases, the extra information can guide your next steps more clearly.
What to expect and how to decide
Ask your clinic how they handle the process. Will your embryos be frozen? How long do the results take? How is the test done, and who explains the findings? The more you understand upfront, the easier it becomes to decide whether NGS is a good fit.
Importance of professional counselling
Genetic testing is personal. It can bring relief, but also uncertainty. That’s why good counselling matters. You should feel supported – not rushed. A clear conversation with your doctor or a specialist can help you sort through the facts and feelings that come with this choice.
Your next step towards parenthood
If you’re considering NGS as part of your fertility journey, the most important step is to stay informed. The more you understand about what’s possible – and what’s not – the easier it becomes to make decisions that feel right for you.
Every situation is different. Some women need clarity after a long road. Others simply want to explore all available options. NGS can offer insight and reassurance – but only if it’s used in the right way, at the right time, with the right support.
If you’re planning treatment abroad, our guide to IVF destinations in Europe can help. It explains where genetic testing is allowed, what to expect in different countries, and gives you a clear overview of how to plan your treatment with confidence. The guide also includes an example of a clinic in Northern Cyprus, including general pricing and success rates – so you know what’s realistic.
Let us help you take the next step with clarity, privacy and support.
Get your guide today or reach out if you’d like more information.